2017-2022/Part 6: Grand Finale
2017: An abrupt ending for teaching community services
After my disastrous start to teaching at TAFE NSW the previous year, I picked up the ball and didn’t stop running for the next three years until I fractured my tibia and fibula in December 2019 just days before the end of semester two (see 2018-2020 below).
Unfortunately, after recuperating from my injuries, COVID-19 prevented any more face-to-face teaching in early 2020 (and beyond) and so I reluctantly called it quits. This was a difficult decision to make, and I didn’t want to complicate my teaching duties and the very long behind the scenes work any more than they already were by taking up digital teaching.
Despite the very long hours I dedicated to teaching, I enjoyed the many challenges that this placed upon me. Had it have not been for the world-wide events of COVID-19, I most likely would still be teaching today.
2018-2020: Operations, non-HIV potential life-threatening conditions
In April 2018 my CD4/viral load was 756/<20, and this was my highest ever count since August 1993. It was long after that time that most HIV clinicians and practices no longer focused on CD4 counts alone, instead focusing more attention on a person’s viral load.
Despite this my HIV Specialist still wanted me to see him twice annually. My viral load results fortunately continued to trend in the right direction thereby being consistently ‘undetectable’. To date my results from April 2018 have failed to be surpassed.
Two years had passed since my heart attack and hernia repair and health wise things couldn’t have been better. This changed suddenly in June 2018 when I needed to have day surgery in hospital for the excision of a small lipoma on my upper back. This was a straightforward procedure, and I suffered no ongoing trauma from it being excised successfully. This was the start of a series of medical interventions by non-elective surgery over the next two and a half years.
Fifteen months later (September 2019) I was experiencing severe lower back pain and my GP sent me for renal ultrasound which revealed that I had a kidney stone in my left kidney. I was then referred to Dr Mark Louie-Johnsun, the urologist that I had been seeing since 2007.
Mark wanted a nuclear medicine test conducted (renal DTPA scan) and two months later it was confirmed that the kidney stone had split into two calculi and moved into an opacified bladder diverticulum (bladder diverticulum identified during a routine endoscopy in 2012). A cystoscopy in early December 2019 resolved this painful situation.
Eleven days later, on 14 December after visiting my mother at Wyong Hospital (where she later died five days later), I was rushing around and slipped on loose gravel and fractured my tibia and fibula. I presented to Wyong Hospital Emergency with my left foot hanging precariously and in agony. Emergency staff put me to sleep while a temporary cast was applied prior to being transferred to Gosford Hospital later that evening. The next day I underwent an emergency fixation of my left tibia and the insertion of an implant consisting of Stryker T2 345mm tibial nail with two distal proximal locking screws. A long rehabilitation followed, and again some more sick leave.
On Monday 3rd February 2020 after graduating from using a walking frame (I couldn’t manage crutches) and being semi-mobile with the aid of a quad walking stick, I had my HIV monitoring done by Dr Kym Collins at her fortnightly HIV/Sexual Health outreach clinic at Wyong Hospital. This was eight months after my last visit with Prof Anthony Kelleher at St. Vincent’s Hospital.
It was during routine discussions with Kym that she suspected that I might have possibly been experiencing a pulmonary embolism (PE). Kym immediately contacted Mariner’s Medical Practice in Tuggerah where I was under the care of my GP, Dr David Burcher. The situation was explained to reception staff however, an appointment was not available until the Wednesday.
David immediately sent me across corridor to Hunter Imaging for a CT scan. After the scan was completed, I was asked to sit in the waiting area for fifteen minutes for the result. A staff member came out and asked me when I was going to see my GP again. When I replied that this depended on my CT result and whether I needed to return to my GP.
With that, the person asking me this realised that my GP was on the same floor as their service and then immediately escorted me across the corridor. The situation was explained to Mariner’s Reception staff, and I got straight in to see David.
David explained my CT result to me and said that it was amazing that I wasn’t feeling extremely unwell as I had extensive bilateral clotting throughout major pulmonary arteries. Blood thinners were prescribed and initially the drug I was prescribed was counteractive to one of the HIV antiretrovirals I was taking. A day later a quick change rectified this situation and three months later there was no further evidence of a PE.
Unfortunately, this was not the end of clots for me and seven months later at suggestion of my cardiologist Dr Andrew Hill (see below), I was sent for a Doppler scan of my left leg because nobody else had thought about doing one after my tibia fracture. Guess what? The doppler revealed that I had a persisting occlusive deep vein thrombosis (DVT) throughout one bifid femoral vein and extending further as partially occlusive thrombus throughout the popliteal vein.
Additionally, a segment of isolated partial thrombus was also identified involving one medial gastrocnemius and webbing noted in another vein. More time on the blood thinning medication was required. Unbeknown to me at the time, because of COVID-19, 31st March 2020 was the last day that dental practices in NSW were permitted to operate before being required to close for three months. Fortunately for me, I was already scheduled to see my Dentist, Dr Trevor Morris at Holdsworth House Dental Practice in Darlinghurst that day.
My appointment was to have broken filling repaired and for Trevor to check out a small ulcer like lesion on the right side of my tongue which had been coming and going for several years and for the past three months was refusing to heal despite the use of a topical oral agent. Trevor repaired my filling and made an urgent appointment for me with an oral surgeon, Dr Bruce Austin at The Vintage in Sussex Street, Sydney later that day. Trevor suspected the lesion was a squamous cell carcinoma (SCC).
Dr Austin couldn’t confirm Trevor’s suspicions and felt that I needed to see a cancer specialist. An appointment was arranged for the following week with Prof Jonathan Clark, a head and neck surgeon at the Chris O’Brien Lifehouse in Camperdown. This marvellous state of the art cancer facility was still seeing and treating patients and not affected by COVIID-19 shutdowns.
Jonathan calmly explained that the tongue lesion was most likely a small tongue cancer and that he favoured doing a wide excision rather than a biopsy/excision. He further explained his rationale and approach that if a biopsy was negative, he still thought that an excision would be warranted to exclude a cancer. My operation for a wide excision of the right tongue took place on 15 April without any complications.
Two weeks later I had a post-operative appointment with Prof Clark, and he said to me “Where you are sitting, you are one of the 10% of patients I see here, that I am very happy to say that your suspected tongue cancer result was negative.” My Pathology results indicated that I had acute inflammation with fungal hyphae and only mild dysplasia (pre-cancerous).
Because of my experience with a pulmonary embolism in early February, my cardiologist Dr Andrew Hill brought forward a routine five-yearly coronary angiogram procedure as a precaution due to evidence of extensive calcification in my left anterior descending (LAD) coronary artery when the CT pulmonary angiography (CTPA) was performed. Thankfully, the procedure confirmed that my LAD was unchanged in appearances following synergy stenting in 2016.
3 September 2020 and another surgical procedure
This time it was a laser enucleation of the prostate. This operation became necessary due to worsening nocturia and associated urine flow problems over thirteen years. I had also been on long-term medication for benign prostate hypoplasia (BPH). The procedure proved to be very effective, and my ‘waterworks’ returned to a normal state and the added benefit of no longer needing to take medication.
The only downside for me was that I fell into the group of men (80%) that experience retrograde ejaculation (dry organism) as a common symptom of having this procedure. There is also a 10% chance that the procedure might need to be repeated in ten years’ time.
In a letter from Prof Kelleher at IBAC at St. Vincent’s to Dr Kym Collins at Holden Street Sexual Health Clinic in Gosford, dated 26 October 2020, it stated in part “I reviewed Paul at the Immunology Clinic today by phone. As you know, he has had a relatively torrid 12 months.”
Shortly afterwards I applied for the Age Pension as I was turning age 66 three months later. My investigations beforehand confirmed that I was eligible for a part pension (due to being in receipt of a Navy & DVA pensions) and could still work part-time if I chose to do so.
2021-2022: Transitioning to final retirement
My birthday came and went as I once again found myself weighing up my options regarding retiring for the final time. I had been employed in the workforce continuously since the age of 15 and wasn’t quite ready to hang up my boots just then. But I was getting close! After considerable thought I decided that I needed to be on the final road to retirement by my 67th birthday.
So, due to staff changes and movements at Holden Street Sexual Health Clinic in Gosford in April 2021, I decided to call it time and commence my extended annual leave/long service leave in November 2021 with my final retirement being officially completed in late November 2022 (see also Talkabout #201, Feb ‘22).
Two months before I resigned in September 2021, I needed to have a routine five-yearly colonoscopy at Wyong Hospital. None of the colonoscopies that I’ve had over the years have detected any cancer or polys. However, on this occasion I was surprised to hear a nurse telling me afterwards in recovery that one polyp had been found.
My Gastroenterologist, Dr John Dowsett confirmed this finding before I left recovery. He told me that he had found a one 1cm typical sessile serrated polyp (SSP) and that had been removed by a new technique known as cold snaring. Dr Dowsett also advised me that due to this finding I would need a repeat colonoscopy in 2024.
Dr Dowsett’s report to my GP further confirmed what he told me verbally in recovery. I was however surprised when reading the last sentence of his report which stated, “Overall therefore significant polyp disease has been found.” I didn’t understand or appreciate that finding only one very small polyp meant that I had significant polyp disease. I queried the wording in the sentence with Dr Dowsett some time later by email. He wrote back a lovely letter confirming that the wording was in fact correct.
2022: Exercise physiology, Remedial massage & Chiro
While I have been transitioning to full retirement, I have taken the opportunity to attend my gym more frequently. In February I was contacted by Vida Health who are partnering with Department of Veteran Affairs (DVA) and offering qualifying veterans the opportunity to participate in one-on-one exercise physiology sessions.
In March I commenced twice weekly sessions (at another gym) and I have benefitted greatly by these, going back to my own gym practising exercises that I have learnt through Vida/DVA. This is one of the best programmes that I have ever participated in and enjoy the two half-hourly sessions.
I have been getting regular remedial massage sessions through my private health fund for the past couple of years at a Chiropractic service in Warner’s Bay. In July my massage therapist recommended I see one of the chiropractors because he suspected I had some upper and lower back issues that couldn’t be resolved by remedial massage alone. He was right and I have been attending regular chiropractor sessions since then and am amazed at the difference it has made to my back. These sessions will end soon as the identified problems were not major and have now been almost satisfactorily resolved.
2022: Taking the bull by the horns
While writing these editions of Talkabout in 2022, several things have occurred and possibly the best of these was finally changing HIV specialists and simplifying my HIV antiretroviral medication after 16 years. I have already written about this to some degree in earlier Talkabout editions (#204 & #205) and will now simply tell readers what happened to reverse earlier decisions made by myself and others in charge of my HIV care.
In May 2022 I contacted Dr David Baker at East Sydney Doctors Practice to see if after eleven years I could be re-treated by him for facial lipoatrophy with ‘Sculptra’ (see Talkabout #203, Jun ’22). David graciously told me that I could still be treated with Sculptra despite it being more than two-years since last having Sculptra injections (subsequent Sculptra treatment can be administered at two-yearly intervals).
He also told me that my previous series of injections all those years ago had served me very well and I was one of the few people living with HIV that this form of treatment had provided excellent results. Despite this, David agreed that I would also benefit further by having two more sessions over two months, and these commenced in June
It was during the second visit for sculptra that I asked David if it was possible to change HIV specialists and become a patient of his at East Sydney Doctors. I also wanted to change HIV antiretrovirals if it was possible. David told me I was welcome to transfer my care if that’s what I wanted.
He didn’t think changing antiretrovirals would be a problem and thought he could simplify my medication regimen. He had two options in mind for going forward which would greatly reduce my daily medication burden. Both options were similar and would do the same job as those that I’d been taking for so long.
I provided David with my own four-page spreadsheet of my HIV history and other supporting documents. He authorised electronic scripts for once daily Symtuza and Dolutegravir on the first of September. My first viral load result on the new medication a month later remained ‘undetectable’. That was almost 6,000 days since commencing my previous multi-medication HIV antiretroviral regimen in 2006.
The whole process of attending East Sydney Doctors in Darlinghurst has been a total change from what I have been used to in the past and I am very pleased to say I have been pleasantly surprised by this. Getting electronic scripts issued and then subsequently getting those scripts filled the same day by a Serafim’s Pharmacy in Darlinghurst is much easier than having to give a week’s notice to a hospital pharmacy on the Central Coast before being able to collect medication .
Subsequent follow-up monitoring in October and December also resulted in ‘undetectable’ viral load results. For the first time in sixteen years my liver function tests (LFT’s) were normal. My regular monitoring frequency has now been stretched out with the next bloods scheduled for March 2023. As I approach my third decade (August 2023) as a person living with HIV, I am very optimistic that the good trend will continue.
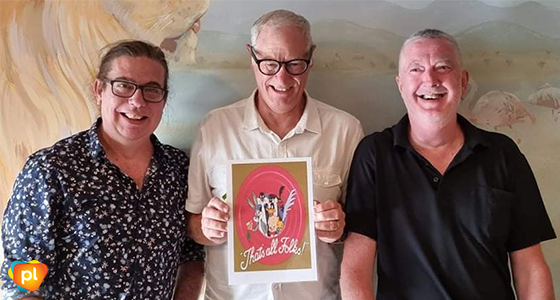
2022: Looney Tunes cartoon character, Porky Pig
This is the last of six instalments that I have written for Talkabout. I have enjoyed revisiting and researching my own HIV lived experiences using my HIV journal (covering the period 1993–2000), other documents, letters and reports which I have collected since 1993. While also re-calling the many events and challenges that I faced over such a long time.
I am conscious of the fact that my story is not special or unique, it’s simply just the way it has panned out for me and how I have chosen to manage and live with HIV. Many others have stories of their own, good, bad or indifferent. I would like to thank Positive Life (NSW) for permitting me the space to put my story into print.
From the outset I have been determined to ‘live’ with HIV and have refused to box myself into a corner and never leaving that corner. I think I have achieved this despite the unique way that HIV/AIDS tends to be so unpredictable. I for one, believe we never know what is around that corner and must be ready for whatever is thrown at us.
I often wish I possessed a crystal ball so that I could see the future and what that future had in store for me. Reality is that I don’t have a crystal ball and that as I continue to age while living with HIV, I hope that I do so without too many more surprises.
Finally, I would like to acknowledge and thank the many health care professionals (either in the NSW Health System and non-government organisations), the many people living with HIV (former work colleagues, clients or friends) that I have had the pleasure to cross paths with in these past 29 years. You are all truly amazing people who have given me a sense of purpose and strength and the will to persevere and to live as best a life as possible over such a long time.
In the famous words of Porky Pig – “That’s all folks!”
Paul R Maudlin OAM, JP
Published in Talkabout #205 May 2023






